Improving How Communities Experience Immunization Services Is Key to Strengthening Demand and Uptake
Published on January 16, 2024

By Lisa Oot and Maia Johnstone, with contributions from Reshma Naik and Lara Vaz
This blog is part of a series on patient, or client, experience of care. It highlights insights, reflections, and resources related to immunization service experience. Visit the MOMENTUM website to read the other blogs and learn more about how MOMENTUM’s insights on experience of care may apply to your own work.
Each year, vaccines for preventable illnesses save the lives of an estimated 3.5 to 5 million children.1 In 2021, global immunization coverage for infants dropped to 81%, the lowest in more than a decade, largely due to the COVID-19 pandemic, conflict, and various health systems challenges.2 While immunization coverage began to recover in 2022, an estimated 20.5 million have not received life-saving vaccines.2
Why are 20 million children still missing out on vaccination?
While numerous issues are at play, one important reason children aren’t being vaccinated is the experience that communities have when interacting with their health system. This experience can create a lasting impression and affect how parents further interact with the health system. For example, when it comes to measles vaccination, caregivers in countries such as Benin, Nepal, and Ethiopia often say that after traveling great distances to bring their children for vaccination, they are asked to wait at the health facility until “enough” children arrive at the session to open the 10-dose vial. If that doesn’t happen, they are sent home without their children having been vaccinated. Other common experiences include being turned away or yelled at by health workers for forgetting to bring the vaccination card; some caregivers then never return with their children to complete the vaccinations, rendering them vulnerable to vaccine preventable diseases.3
Effective Immunization Requires More Than Outreach
These experiences illustrate clearly that reaching children with immunizations requires much more than having vaccines in stock and letting people know about them. They also underscore the importance of giving attention to the service experience, which includes “factors within and beyond the interaction between health worker and client which affect the delivery and experience of the immunization service”.4
As described in the Vaccination Demand HUB, the immunization service experience considers various elements that affect clients and health workers. These elements contribute to whether a client has a positive, high-quality experience during an immunization visit that is centered on their needs.4 Figure 1 highlights how experience of care fits into the immunization journey, both as its own step and interconnected with other stages along the journey to health and immunization. The way clients are treated by health workers, how satisfied they are with services, the trust built between them and health workers, and the physical space designated for immunizations are all factors that may affect the experience of those seeking services.5 Equally important are health workers’ experiences, how well they are trained, and how equipped and supported they feel to deliver immunization services.5
Applying the Journey to Health & Immunization Framework
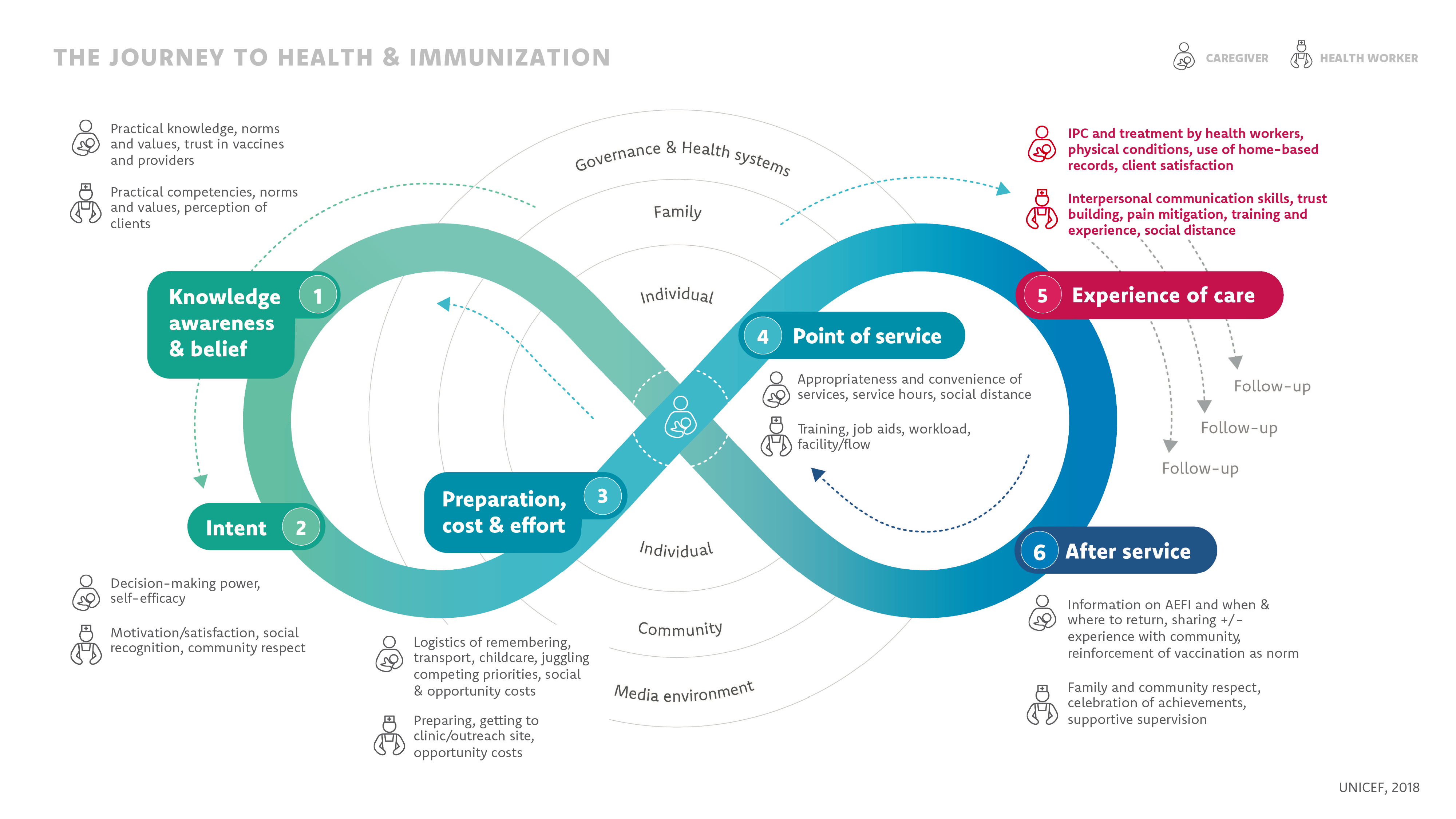
As with other types of health services, health workers who provide immunizations require consistent, adequate supplies to do their work well. Frequent stockouts of vaccines or other equipment can affect how communities trust and view the health system.4And like child health services more broadly, for immunization, we are often talking about the experience of a caregiver or accompanying person, rather than the child, though a caregiver’s experience may include how they perceive their child was treated. Completing the immunization schedule requires repeating the journey to health and immunization several times, so a positive—or poor—experience during any one visit can strongly influence a caregiver’s willingness to return so their child receives all doses of the live-saving vaccines they require.4
Immunization service experience considers both the health provider and the caregiver, and the factors that influence providers’ abilities to provide person-centered, high-quality care (see the first blog in this series for more on person-centered care). For many marginalized and/or hard to reach populations, immunization services may be the only health services they can access. This reality makes it even more critical to ensure that every experience, whether at a facility, with traveling mobile teams, or through outreach, is positive, and that these communities are brought into the health system not only for immunization, but also for their other health needs. Equally important, health workers must have the necessary tools, supplies and support to be able to address those comprehensive health needs.
Moving the Needle: Research and Programming from MOMENTUM
Fostering empathy among health care providers and supporting them to deliver person-centered care are important parts of improving clients’ immunization service experience. MOMENTUM Routine Immunization Transformation and Equity partners with health systems staff and community members in an array of countries, from Serbia, North Macedonia, and Moldova in Eastern Europe to countries across Africa, to implement novel approaches focused on strengthening provider and community engagement and person-centered care.
In Eastern Europe, the project is working with medical doctors, nurses, and pharmacists to increase demand and uptake of COVID-19 vaccination by ensuring health providers are prepared to engage clients with the appropriate knowledge and information and to facilitate positive provider-patient interactions. During positive interactions, providers encourage patients to adopt an appropriate behavior like getting the COVID-19 vaccine while also focusing on patients’ needs, situations, motivations and abilities. This effort is being carried out through a one-day, in-person, continuous medical education course focused on integration of COVID-19 vaccination as part of a healthy lifestyle and tailored to context.6 The course seeks to enhance the skills of medical professionals who work with high-risk populations like pregnant women and older adults living with chronic disease to ensure they feel comfortable and confident about vaccination. Aligned to the Journey to Health and Immunization Framework, this work aims to address aspects like health worker empowerment and perception of service experience, which can contribute to a positive experience of care.

The project’s study in the Democratic Republic of the Congo (DRC), Mozambique, and Nigeria highlights barriers that caregivers and providers face, as well as systemic challenges to fully vaccinating children. One important finding is that power dynamics play an important role in how immunization services are delivered. For example, in some of these settings, health workers held relative privilege and wielded power over clients; however, their managerial and institutional superiors simultaneously made them feel disempowered and undervalued. These complex experiences and power dynamics can result in disrespectful care as health workers strive to provide services in situations that they themselves find challenging.7 The findings also showed that while caregiver reports of service quality varied across those interviewed, mothers of under-vaccinated children were likely to report poor service experience as a reason for not returning.7
This multi-country research informed co-creation workshops that brought health workers and community members together using tools from human-centered design (HCD) and the Journey to Health and Immunization Framework. During these workshops, participants used vignettes—short stories developed by the research team using synthesized, non-identifiable data that centered around caregivers’ experiences—to illustrate common immunization challenges. Vignettes included Caregiver facing multiple intersecting and interacting barriers based on her context and Immunization services not aligned with a caregiver’s needs.
The co-creation workshops were effective in using identified barriers and drivers of vaccination and in creating the space for community and health system participants to come together as equals—a new experience for participants—to propose solutions to those problems. Many solutions reflected ideas on people-centered care and improved service experience, like integrating delivery of all child health services at facilities and reducing wait times.7 Integral to achieving a positive, quality, person-centered experience is creating opportunities to enhance community voice, input, and demand for vaccination, essential components of person-centered immunization service experience and align to the Journey to Health and Immunization Framework.4, 5 The project enhanced community voice, input, and demand through its application and use of HCD processes like the co-creation workshops and vignettes.
Each year, vaccines for preventable illnesses save the lives of an estimated 3.5 to 5 million children.
What More Is Needed to Improve Immunization Service Experience?
There is growing recognition that service experience plays an important role in strengthening demand for vaccination services and ensuring that every child is fully vaccinated or has received all required doses. One important next step for the field is to determine a set of standard metrics that help countries monitor and measure various components across service experience, building on the World Health Organization’s work to understand the behavioral and social drivers of vaccine uptake. Many countries already have data available that can be triangulated, analyzed, and interpreted to better understand their specific contextual issues related to the service experience and what is needed to address them. Moreover, bolstering efforts to engage communities themselves in designing, implementing, and monitoring services can lead to additional improvements in their quality and reach. This could include engaging communities in the microplanning process or implementing integrated community and health worker Quality Improvement Teams that include non-health stakeholders in supervision visits to understand the value of their investment in immunization.
Work by MOMENTUM and Breakthrough RESEARCH have found that inequitable power structures within health systems, like providers feeling disempowered, can affect the delivery of people-centered care and can have consequences, including clients experiencing disrespectful care.7, 8 MOMENTUM’s work shows there is interest and commitment within communities and health systems to improve the service experience. Ways forward include orienting primary health care around health provider and user needs and investing in programs that are gender-responsive and people-centered, integrated with HCD and intersectional lenses, and explicitly address institutional and structural root causes. Policymakers and funders can build on this evidence to provide the guidance and resources needed to advance such efforts.7
Finally, as with other health services, more research is needed to understand provider perspectives and the ecosystems in which they work. Alongside clinical training and skills, providers need motivation and a supportive infrastructure—like a clean health facility in which to work, timely salary payments, a clear system and opportunities for advancement and collaboration with other health service providers, and recognition for their work—to enable them to consistently provide high-quality care.
To learn more about patient experience of care, check out these useful resources!
Photo caption: Nurse Rose Lueji organizes vaccination records at the Munigi Health Center in Goma, Democratic Republic of the Congo. Photo Credit: Crystal Stafford, Corus International
References
- World Health Organization. Vaccines and Immunization.
- UNICEF. (2023). Immunization.
- Castle, N., et al. 2023. Using the Journey to Health and Immunization (JTHI) Framework to Engage Stakeholders in Identifying Behavioral and Social Drivers of Routine Immunization in Nepal.
- Vaccination Demand Hub. Service experience.
- UNICEF. (2018). Journey to health & immunization framework in, Demand for health services field guide: a human-centered approach. New York: UNICEF.
- MOMENTUM. (2023). MOMENTUM projects in Europe, Eurasia, and the Middle East: Regional reference brief. Washington, DC: USAID MOMENTUM.
- Shearer, Jessica C., Nava, Olivia, Prosser, Wendy, Nawaz, Saira et al. 2023. Uncovering the drivers of childhood immunization inequality with caregivers, community members and health system stakeholders: Results from a human-centered design study in DRC, Mozambique and Nigeria. Vaccines (Basel) 11(3): 689.
- Sripad P, Peterson S, Idrissou D, et al. 2023. Applying a power and gender lens to understanding health care provider experience and behavior: a multicountry qualitative study. Glob Health Sci Pract. 113): e2200420.

