The “How” of Person-Centered Care in Family Planning: New Tools for Private Provider Service Delivery
Published on September 30, 2024

By Alexandra Angel, Rebecca Husband, and Pierre Moon, MOMENTUM Private Healthcare Delivery with contributions from Colby Reed, MOMENTUM Knowledge Accelerator
This blog, part of a series on patient experience of care, highlights insights, reflections, and resources related to person-centered care. Visit the MOMENTUM website to read other blogs in the series and learn more about how insights from MOMENTUM’s experience of care work may apply to you.
Putting people at the center of health care, focusing on their perspectives and preferences, has long been embraced as best practice in family planning and maternal-child health services. Yet, making this a reality for people worldwide remains an urgent priority. With growing recognition that person-centered care (PCC) improves all health care— highlighted by the World Health Organization in 2016 and by a Lancet Commission in 2018 – there is great opportunity in the next decade to advance PCC around the world.1-2 New movements supporting individuals to manage their own health care, such as through self-care and digital health interventions, have added momentum to the PCC movement, while also elevating the need to link such clients to supportive, person-centered health systems.3
There is general consensus that PCC approaches can lead to healthier people, but agreeing to advance PCC as a global goal is only the first step. Determining how the global health community will define, measure, evaluate, and integrate PCC across different levels of the health ecosystem—and developing the validated tools, standards, and guidance to operationalize it—are the critical next steps that must follow.4
Applying PCC to Family Planning and Reproductive Health in the Private Sector
The evolving definition of PCC is partially attributed to its variability across different health domains, despite the common goal of improving client experience of care and overall health outcomes.5 In the HIV/AIDS community, for example, PCC integration may focus on stigma reduction interventions and individually tailored treatment adherence strategies. In maternal health, PCC is delivered through a respectful maternity care approach by assuring “dignity, privacy and confidentiality…freedom from harm and mistreatment…informed choice and continuous support during labor and childbirth.”6 For family planning and reproductive health (FP/RH), PCC is an intrinsic part of a rights-based approach that recognizes the individual’s right to choose whether, when, and how many children to have.7 PCC in FP/RH at the service level may include a focus on the provision of unbiased, accurate information and the reduction of provider judgment or coercion around method choice.
The private sector is an important part of making person-centered FP/RH services a reality, as roughly one-third of modern contraceptive users in low- and middle-income countries (LMICs) regularly access their method from private providers.8,9 Yet private sector providers in these countries often miss out on the guidance, certification, and continuing education opportunities available to their public sector counterparts. Private providers are also commonly left out of conversations about PCC that may be percolating in LMIC public sectors. Staff attrition (common in the private sector) and concerns about missed income when participating in in-service training opportunities result in private providers being less likely to benefit from new clinical and technical approaches. Failing to incorporate the capacity strengthening needs of private FP/RH providers in operationalizing PCC is a missed opportunity to support an improved experience of care for their clients. When private sector providers are fully equipped to deliver high-quality, person-centered FP services, clients can feel confident to make the reproductive health choices that respond to their needs and expectations.

Moving the Needle: How MOMENTUM Is Helping Private Providers Deliver Person-Centered Care
MOMENTUM Private Healthcare Delivery is addressing the lack of PCC guidance and training opportunities for private sector providers in LMICs by developing tools to help integrate PCC within health facilities. The Person-Centered Care Toolkit for Family Planning/Reproductive Health and Maternal, Newborn, and Child Health, intended for use by program implementers and managers overseeing networks of private providers, orients users to the broad concepts of PCC within both FP/RH and maternal, newborn and child health care (MNCH). The toolkit lays out practical guidance for centering care and services on the values, preferences, and needs of the individual coming for services.
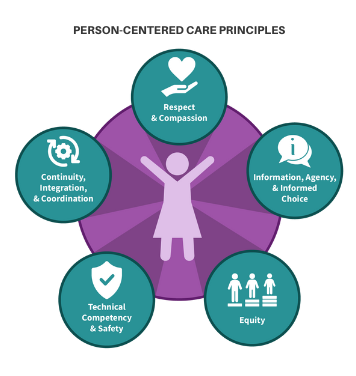
The PCC toolkit is organized around five guiding principles, aligning with common understandings of PCC and quality care as defined by the World Health Organization (WHO) and Institute of Medicine10 (see Figure 1). These principles underpin a suite of core training modules and management resources that enable local private sector actors, from managers and supervisors to providers and facility staff, to translate PCC concepts into facility-level behaviors and practices. Training modules within the toolkit draw upon evidence-based practices and include content on adolescent- and youth-responsive care, gender transformative care, respectful maternity and child care, client-centered FP counseling using Counseling for Choice, and communicating with empathy. While the rationale for this resource is to provide information and training materials for private providers, the content could be used or adapted by public sector actors.
In September 2023, a team in Benin used the PCC toolkit to facilitate training for over 170 owners, providers, and staff across 40 private health facilities. MOMENTUM Private Healthcare Delivery is conducting a study assessing the acceptability and feasibility of implementing the PCC toolkit with private FP/RH and MNCH providers. The study also examines the toolkit’s effectiveness in improving client experience of care, using existing measurement tools (see Box 2); the study ends in September 2024.
Preliminary study results show that the PCC toolkit’s concepts and resources have shifted the perspectives of supervisors and providers on how they deliver care. Study participants are demonstrating a nuanced grasp of what it means to offer PCC. One participant illustrated their understanding using the example of a client presenting with hypertension as a complication:
“We have got to get the patient to explain her experience. Apart from the other standard parameters that we know can induce hypertension, there are things that can be linked to her daily life and which can be at the root of this hypertension. And by managing and resolving this [root] problem, we can avoid administering [unnecessary] medication…not all individuals are the same […] there are other factors that have influence.”
Another study participant gave the example of how using the Counseling for Choice approach helps them center their care around their FP clients:
“When we try to have a good discussion [using Counseling for Choice] with them [the clients], we give them explanations, they understand, and they participate in the care.”
In recent years, several measurement tools for PCC have been used by the FP/RH community of practice. Among them are the seminal scales developed by Patience Afulani and May Sudhinaraset for FP/RH and maternity care.11 These scales comprise roughly 20 to 40 questions each and aim to measure the client’s experience of PCC for the specific health area. While these scales can produce meaningful, actionable results, they are too lengthy to be easily integrated into routine monitoring, client feedback, and supervision systems. Other shorter-form scales exist, but they also focus on just one specific health area. The Lancet recently highlighted that more work is needed to rigorously measure the implementation of PCC approaches, but the community lacks a validated PCC scale that can both integrate into monitoring systems and accurately assess the person’s experience regardless of service provided. Given areas of overlap between FP/RH and MNCH services, MOMENTUM is developing and testing a single 7-10 item scale to measure patients’ experience of PCC across FP/RH and MNCH. The new scale, informed by previous tools, is being used as part of the study in Benin. Once validated, it will offer implementers a way to measure PCC across services as countries increasingly adopt comprehensive PCC approaches to care.
What More Is Needed?
The PCC toolkit addresses an existing gap in the FP/RH community by providing a comprehensive resource to introduce PCC approaches at the facility level. Importantly, it translates the abstract principles and concepts behind PCC into specific skill sets and practices, focusing on behavior change among providers and their supervisors. For example, providers will gain skills in cultivating emotional intelligence, in gender transformative and respectful care practices, and in how to serve young people with a PCC approach. Results from the MOMENTUM study in Benin will help validate the toolkit and add to the evidence base on how provider-facing interventions enhance PCC and improve client experience of care. Though focused on select health areas, the principles and practices within the PCC toolkit help providers foster a person-centered mentality that could be applied to other primary health care services offered within a facility.
MOMENTUM Private Healthcare Delivery’s work primarily focuses on the staff behaviors and competencies required to operationalize PCC, but this is only one element of the bigger PCC picture. Effective models and guidance on the how of PCC are needed at multiple levels of the health ecosystem—not just for FP/RH, but for primary health care in general. For example, what policies are essential to make PCC successful? How should providers and systems be held accountable for implementing PCC approaches? How much does operationalizing PCC across a health system cost? While the global health community continues to advance and advocate for PCC around the world, these and many other important questions will need to be explored. For now, the PCC toolkit offers tangible guidance and tools designed for facility-level managers and providers to meaningfully improve an individual’s experience of their FP/RH care, whether they seek their service in the public or private sector.
To learn more about PCC, check out these additional resources:
- Counseling for Choice
- Quality of Care for Family Planning: A Comparison of Private and Public Facilities in Seven Countries Using Survey Data
- Person-Centered Family Planning Counseling in the Private Sector
References
- World Health Organization. (n.d.). Integrated people-centred care.
- Kruk, M. E., Gage, A. D., Arsenault, C., Jordan, K., Leslie, H.H., Roder-DeWan, S., Adeyi, O., Barker, P., Daelmans, B., Doubova, S. V., English, M., García-Elorrio, E., Guanais, F., Gureje, O., Hirschhorn, L. R., Jiang, L., Kelley, E., Tekle Lemango, E., Liljestrand, J. … Pate, M. High-quality health systems in the Sustainable Development Goals era: Time for a revolution. The Lancet Global Health, 6(11): e1196–e1252. https://doi.org/10.1016/S2214-109X(18)30386-3
- World Health Organization. (2021, June 23). Putting people first in managing their health: New WHO guideline on self-care interventions. https://www.who.int/news/item/23-06-2021-putting-people-first-in-managing-their-health-new-who-guideline-on-self-care-interventions
- Duong, D. B., Holt, B., Munoz, C., & Pollack, T. M. (2024). For and with people: Announcing the Lancet Global Health commission on people-centered care for universal health coverage and a call for commissioner nominations. The Lancet Global Health, 12(7): e1089–e10902024. https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(24)00216-X/fulltext?dgcid=raven_jbs_aip_email
- Grover, S., Fitzpatrick, A., Tabassum Azim, F., Ariza-Vega, P., Bellwood, P., Burns, J., Burton, E., Fleig, L., Clemson, L., Hoppmann, C. A., Madden, K. M., Price, M., Langford, D., & Ash, M. C.Defining and implementing patient-centered care: An umbrella review. Patient Education and Counseling, 105(7): 1679–1688.World Health Organization. (2018). WHO recommendations: Intrapartum care for a positive childbirth experience. https://www.ncbi.nlm.nih.gov/books/NBK513809/
- U.S. Agency for International Development. (2024). Pathways to progress for sexual and reproductive health. https://www.usaid.gov/sites/default/files/2024-04/PRH%20USAID_2024_Global_Health_PRH_Pathways_Report-FINAL_508.pdf
- Roles of the public and private sectors in providing contraception and how they can best collaborate to expand contraceptive access and choice (shopsplusproject.org). https://shopsplusproject.org/sites/default/files/resources/Sources%20for%20Family%20Planning%20in%2036%20Countries-Where%20Women%20Go%20and%20Why%20it%20Matters.pdf
- Bradley, S. E. K. & Shiras, T. (2020). Where women access contraception in 36 low- and middle-income countries and why it matters. Sustaining Health Outcomes through the Private Sector Plus Project. https://pubmed.ncbi.nlm.nih.gov/36332074/
- Agency for Healthcare Research and Quality. (2022, December). Six domains of healthcare quality. U.S. Department of Health and Human Services. https://www.ahrq.gov/talkingquality/measures/six-domains.html
- Sudhinaraset, M., Afulani, P. A., Diamond-Smith, N., Golub, G., & Srivastava, A. (2017). Development of a person-centered family planning scale in India and Kenya. Studies in Family Planning 49(3):237–258. https://pubmed.ncbi.nlm.nih.gov/30069983/
- Afulani, P.A., Diamond-Smith, N., Golub, G., & Sudhinaraset, M. (2017). Development of a tool to measure person-centered maternity care in developing settings: validation in a rural and urban Kenyan population. Reproductive Health, 14 (118). https://doi.org/10.1186/s12978-017-0381-7

