A Perfect Match: A Journey of Love and Primary Health Care in Eastern Indonesia
Published on January 10, 2025
The piece below originally appeared on USAID Exposure. Read the original piece here.
Siprianus first laid eyes on Angeliana when she popped up under “people you might know” on Facebook. He was studying accounting in university on a nearby Indonesian island. She was studying biology in eastern Indonesia.
After five years of digital courting, they met in person in December 2022 — and married soon after. Angeliana found out she was pregnant a few months later.

Starting at Birth
In Indonesia, Angeliana and Siprianus live in a designated “Desa Siaga” — or prepared primary health care (PHC) community — on Flores Island, East Nusa Tenggara. In a Desa Siaga, USAID partners with village leaders and the Ministry of Health to ensure that communities are prepared to support healthy pregnancies and safe deliveries. The Desa Siaga model, first developed by USAID 20 years ago, is part of Indonesia’s Integrated Primary Health Care program, which focuses on delivering quality care throughout a person’s life.


Vital Village Midwives
Throughout Angeliana’s pregnancy, the village midwife and a kader, or community health worker, visited Angeliana and Siprianus monthly to discuss healthy behaviors for her and her baby and how to identify early signs of potential complications. Village midwives like Yhanista M.A.D. Lewis are an integral part of PHC as they meet the basic health needs of all members of the community as well as form a linkage to higher level care at the nearby Puskesmas.
“Every village needs at least one midwife,“ Yhanista said. “Village midwives focus on maternal and newborn health, but we also focus on the elderly and NCDs (noncommunicable diseases). The village relies on us.”



A Swift Response
When Angeliana’s water broke weeks before her due date, Siprianus called the village midwife and kader, and immediately alerted the community ambulance — in this instance, a neighbor who had agreed to serve the community in case of emergency.


They were transported to the nearby puskesmas, or community health center, which ensures that primary health care is delivered near the community. This is where mothers like Angeliana bring their babies to check on the health of mom and baby before, during, and after the baby is born.


The Right Referral
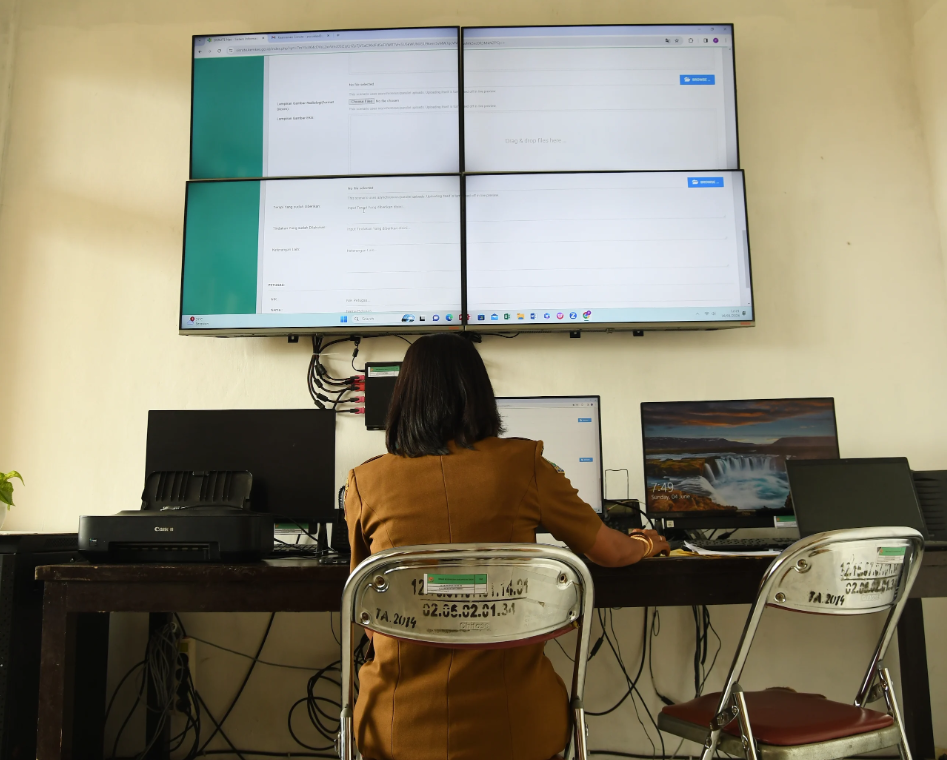
After being closely monitored for nearly eight hours, the on-call doctor decided to make an emergency referral to the nearby TC Tiller Hospital. The team entered Angeliana’s information into Sistem Informasi Rujukan Terintegrasi Nasional, or SISRUTE, an emergency referral system that automatically triggered an alarm at the referred hospital so the team there could prepare for Angeliana’s arrival. Angeliana and Siprianus were transported in the Puskesmas ambulance. Their entire family followed behind.
The team at the regional referral hospital, TC Hiller Hospital, was more than prepared — since June 2022, they had been receiving training from USAID for maternal and neonatal emergencies. After initial visits from mentors from another hospital, the pediatrician and obstetrician at TC Hiller became mentors themselves and now mentor the hospital midwives. The medical team conducts monthly drills to build preparedness and confidence for workers who will respond to childbirth emergencies.



Delivery Due Date
After checking Angeliana’s progress, the staff determined they needed to induce labor. Thirty-six hours later, their son was born.
Alexa B. D. Bela, the kader, waited with them the whole time, “because it’s my responsibility to make sure she is safe.”
Siprianus adds: “I am very satisfied with all of the health workers. They kept accompanying us and giving us information. We never had to worry. All of our questions were answered.”



Planning Ahead
Chrisantos Gani is the first boy in the family and receives lots of love and attention from his extended family. His middle name is a combination of Siprianus GA[lis] and Angeliana NI[ta]. After Angeliana delivered Chrisantos, she opted to have a family planning implant inserted.
She likes that she doesn’t have to do anything, and since it lasts for three years she’ll have time to find a job and use her biology degree before she and Siprianus think about growing their family.
As for Chrisantos, Angeliana hopes he will have the freedom to choose his own future. Siprianus jokes, “I want him to become a nurse so he can take care of us when we’re old and sick.”

This story highlights USAID’s partnership with village leaders and the Ministry of Health in Indonesia to ensure that primary health care systems are prepared to support the delivery of healthy babies to decrease maternal and child mortality. The U.S. Government has made a number of high-level commitments to address maternal and child mortality through primary health care (PHC) and Primary Impact, and the Global Health Worker Initiative.
Narrative and photos by Amy Cotter Fowler for USAID.

